Suicide Prevention Must Include Fathers: Why Paternal Mental Health Can No Longer Be Overlooked
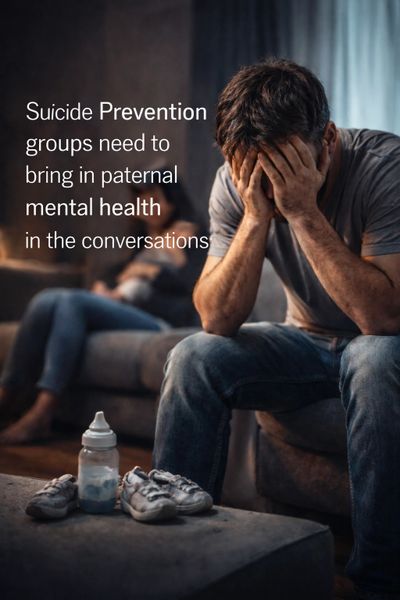
Across the UK and internationally, suicide prevention has rightly become a major public health priority. Governments, charities, health systems, and community organisations are investing in awareness campaigns, crisis support, early intervention, and research. Yet one critical area still remains under-recognised in many suicide prevention strategies: paternal mental health, particularly during pregnancy and the early years of a child’s life.
Emerging research, including recent population-level data from Wales, shows that fathers are dying by suicide at significantly higher rates than mothers during the first 1,001 days (pregnancy to age two). This period is widely recognised as one of the most sensitive stages of family development, yet fathers often remain invisible within assessment pathways, support systems, and prevention strategies. If suicide prevention is to be truly effective, it must include fathers not as an afterthought, but as a central part of family mental health planning.
Fathers are often present — but not identified
Many suicide prevention programmes operate through healthcare contact points such as maternity services, GP appointments, or early years support. While mothers are routinely screened for mental health difficulties, fathers are rarely asked even the most basic wellbeing questions. This is not because fathers are unwilling to talk — in many cases they simply are not asked, not recorded in systems, or not considered part of the clinical pathway.
This creates a major prevention gap. The transition to parenthood brings profound psychological, social, and financial pressures for many men: identity changes, relationship adjustments, sleep deprivation, work stress, financial strain, and the emotional impact of supporting a partner who may also be struggling. When these pressures combine with previous trauma, mental health history, or lack of support networks, vulnerability can increase significantly.
Suicide prevention must become family-inclusive
Traditional suicide prevention models often focus on individuals in isolation. However, the perinatal period is a family transition, and prevention approaches must reflect that reality. Supporting fathers is not about shifting attention away from mothers; it is about recognising that family wellbeing is interconnected. When fathers are supported, outcomes improve not only for them, but also for mothers, children, and the stability of the family environment.
Family-inclusive suicide prevention strategies could include:
- Routine mental health check-ins for fathers during maternity and early years contacts
- Training frontline professionals to recognise paternal distress signals
- Father-inclusive parenting, relationship, and wellbeing programmes
- Workplace awareness initiatives for new fathers
- Community-based peer support groups specifically designed for dads
- Data collection systems that record paternal wellbeing, not only maternal outcomes
These steps are practical, achievable, and evidence-informed — yet many services still operate without them.
Breaking the silence around paternal distress
One of the most significant barriers is cultural. Many men still feel pressure to “stay strong,” particularly when a new baby arrives. They may believe their role is to support others while ignoring their own wellbeing. Without visible messaging that fathers’ mental health matters, many struggle quietly until difficulties escalate.
Suicide prevention messaging must therefore evolve. Campaigns that speak directly to fathers, highlight emotional transitions into fatherhood, and normalise help-seeking behaviour can make a measurable difference. When men see themselves reflected in prevention messaging, engagement increases.
A systems issue, not an individual failure
It is important to recognise that the lack of paternal inclusion is not the fault of individual professionals or services; it is largely the result of historical system design. For decades, perinatal mental health policy and service frameworks were built almost exclusively around maternal outcomes.
While this focus was essential and remains critically important, modern evidence now clearly shows that supporting fathers is also prevention.
When suicide prevention groups expand their frameworks to include paternal mental health, they strengthen — not dilute — their impact. Prevention becomes earlier, more comprehensive, and more family-centred.
The way forward
The growing evidence base presents a clear opportunity. Suicide prevention organisations, health boards, policymakers, and community groups can begin integrating paternal mental health into their strategies immediately. This does not require building entirely new systems; it often involves small but powerful changes: asking fathers how they are, including them in assessments, providing targeted resources, and ensuring services are visibly welcoming to men.
Suicide prevention cannot succeed if large groups of at-risk individuals remain unseen. Fathers are present at antenatal appointments, present in delivery rooms, present in homes supporting their partners and children — yet too often absent from prevention frameworks.
If we are serious about reducing suicide rates, protecting families, and strengthening early-years outcomes, paternal mental health must become part of every suicide prevention conversation. Supporting fathers is not an optional extra. It is prevention, early intervention, and family protection combined.
References
Swansea University (2025). Study exposes hidden crisis of suicide among new fathers. Swansea University Press Office.
1001 Critical Days Foundation (2025). World-first research exposes hidden crisis of suicide amongst new dads.
ADhd and Perinatal Mental Health
ADHD in Adults: A Late Recognition with Early Family Implications - perinatal mental health
“Recognising ADHD in parents early is not only about diagnosis — it is about prevention, family stability, and giving children the strongest possible start.”
In 2015 I wrote about ADHD and perinatal mental health in , highlighting overlooked parental mental-health needs. - link https://www.huffingtonpost.co.uk/markwilliams/adhd-and-perinatal-mental-health_b_7077498.html
For decades, ADHD was widely considered a childhood condition — something that children “grew out of” or that only affected boys who struggled in school. It was not until the mid-2000s, particularly following the publication of the UK NICE ADHD guidelines (2008), that adult ADHD began to receive serious recognition in clinical pathways.
Prior to this, many adults — including thousands of parents — lived with undiagnosed ADHD, often experiencing anxiety, depression, relationship stress, and difficulties with emotional regulation without understanding why.
Today we know that ADHD is a lifespan neurodevelopmental condition, and growing awareness of adult ADHD is changing how we think about mental health across the entire family system — particularly during the perinatal period, one of the most psychologically demanding stages of adult life.
The hidden generation of undiagnosed adults
Many adults who are now in their 30s, 40s, 50s and beyond were never assessed as children, because diagnostic awareness, screening systems, and professional training were limited. As a result, large numbers of people entered adulthood carrying challenges that were often mislabelled as personality issues, anxiety disorders, depression, or behavioural problems.
For parents, this lack of recognition can have significant consequences. Pregnancy, birth, and early parenting bring profound lifestyle changes — disrupted sleep, increased responsibility, financial pressure, relationship adjustments, and emotional strain. For someone living with undiagnosed ADHD traits such as executive-function difficulties, emotional dysregulation, impulsivity, or sensory overload, these changes can significantly increase vulnerability to mental health challenges.
Research increasingly shows that parents with ADHD are at higher risk of perinatal anxiety, depression, burnout, and relationship strain, particularly when support systems are limited or when services focus only on one parent.
Historically, perinatal mental health services were designed primarily around mothers’ needs, but understanding is now expanding toward whole-family mental health, recognising that both parents’ psychological wellbeing shapes child outcomes.
Why early recognition matters for families
When ADHD is identified early — ideally before or during pregnancy — parents can access education, coping strategies, medication reviews where appropriate, and practical support that significantly reduces stress. Early recognition allows individuals to understand their cognitive style rather than internalise years of self-criticism or perceived “failure,” a shift that alone can reduce anxiety and depressive symptoms.
Preventive, family-focused approaches can include:
- Psychoeducation for parents about ADHD and emotional regulation
- Planning for sleep disruption and routine changes after birth
- Practical executive-function supports (reminder systems, structured routines, shared task planning)
- Couple-based communication support
- Workplace adjustments during pregnancy and early parenthood
- Parenting programmes tailored for neurodivergent parents
When these are in place, the perinatal period becomes more manageable and less overwhelming, reducing the likelihood of crisis-level mental health needs.
Prevention: protecting both parents’ mental health
The perinatal period is one of the strongest windows for mental-health prevention. Anxiety and depression at this stage can affect bonding, parental confidence, relationship stability, and long-term family wellbeing. Supporting parents with ADHD — diagnosed or suspected — acts as a protective factor for the entire family system.
Often, simple adjustments such as clear communication, written care plans, flexible scheduling, neurodiversity-aware screening, inclusive support for both parents, and peer networks can significantly reduce stress and improve engagement with services.
It is also important to recognise that parents may experience dual or multiple diagnoses, and ADHD does not exist in isolation. Some mothers who have experienced postpartum psychosis have later been identified as having ADHD, although this represents only one possible factor among many.
Postpartum psychosis is a complex condition influenced by biological, psychological, and social factors and can affect any parent, including fathers and partners. Recognising underlying neurodiversity where it exists may help some parents access more tailored long-term support, but it should always be understood within the wider context of comprehensive perinatal mental health care.
Recognising ADHD in parents also supports earlier understanding of children’s developmental pathways.
Given ADHD’s strong heritability, parental awareness enables earlier support where needed, reducing longer-term educational, emotional, and behavioural risks.
A shift toward whole-family perinatal mental health
Mental health care is gradually moving away from individualised models toward family-centred prevention. When one parent struggles, the impact is felt across the household. When both parents are supported, children benefit from stability, secure attachment, and improved developmental outcomes.
Recognising adult ADHD is therefore not just a diagnostic step — it is a public-health opportunity to reduce anxiety, depression, relationship strain, and long-term mental-health costs.
Looking forward
Despite progress since the late 2000s, many parents remain undiagnosed or unsupported. Assessment waiting lists remain long, and perinatal services do not yet consistently screen for neurodiversity.
The future of perinatal mental health lies in early recognition, inclusive services, and preventive family support. When parents are understood rather than judged, they are far more likely to thrive during one of life’s most demanding transitions — benefiting mothers, fathers, partners, and children alike.
Personal reflection
As a father diagnosed with ADHD after my son was born, many lifelong struggles suddenly made sense. Parenthood intensified those challenges, but diagnosis brought understanding, practical strategies, and self-compassion.
Early recognition of parental ADHD can reduce anxiety, depression, and relationship strain, helping families navigate the perinatal period with greater confidence and stability.
References (selected)
- National Institute for Health and Care Excellence (NICE). (2008; updated 2018). Attention deficit hyperactivity disorder: diagnosis and management (NG87).
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
- Paulson, J.F. & Bazemore, S.D. (2010). Prenatal and postpartum depression in fathers. JAMA.
- Ramchandani, P. et al. (2008). Paternal depression and child development. The Lancet.
- Darwin, Z. et al. (2017). Fathers’ mental health during pregnancy and the first postnatal year. BMC Pregnancy and Childbirth.
- Faraone, S.V. & Larsson, H. (2019). Genetics of ADHD. Molecular Psychiatry.

What I Heard at LSE About Maternal Mental Health — and Why Fathers Can’t Be Ignored
Last week I attended #MaternalPsychologicalWellbeing: A Challenge and a Unique Opportunity at LSE in London.
I wasn’t there to speak — I was there to listen, reflect, and act.
One moment that stayed with me was hearing Adrienne Burgess from the Fatherhood Institute explain that during the perinatal period, for every one mother who dies by suicide, around seven fathers also die. That statistic landed heavily in the room — and it should. These are not abstract numbers; these are families.
My role on the day was simple but intentional: to put information directly into the hands of people in the room who have the power to make change. Leaflets, conversations, and quiet challenges — reminders that fathers and partners must not be invisible in this space.
I’ve worked in general mental health for over 20 years, including 16 years in perinatal mental health, and I’ve often noticed how support can become focused on one parent.
This feels very different from many other areas of mental health, where care is more naturally wrapped around families and relationships, with early support offered before difficulties escalate.
What was clear from the discussions is that services are growing — but families are still being failed.
I’ll say this again, as I always do:
there is no one who knows a mother better than her partner and close family. They are often the first to notice changes, the first to worry, and the first to feel powerless. If we equip them with the right tools, language, and confidence, they can help families engage with support early and at a low level, long before things reach crisis point.
Supporting mothers means supporting families.
Supporting families means including fathers — not as an afterthought, but as part of the solution.
Just a idea -
Early, low-level contact
A health visitor or community worker checks in early, not just at crisis point
Support is framed as normal and preventative, not clinical or alarming
No long waits, no complex thresholds
Partner and family included
The partner is actively invited into conversations
They’re asked: “What are you noticing? How are you coping?”
Practical guidance is given on how to support emotional wellbeing day-to-day
Wider family (where appropriate) are signposted too
Wrapped, not siloed
Mental health, physical health, parenting, finances, sleep, and relationships are seen as connected
One named worker coordinates support so parents aren’t repeating their story
Clear pathways if things worsen — no sudden drop-offs
Strengths-based, not deficit-based
Focus isn’t just on symptoms, but on what’s already working
Parents are treated as partners in care, not problems to be fixed
Cultural, neurodiversity, and family differences are respected
Escalation only when needed
If mental health deteriorates, support steps up smoothly
Because trust already exists, families are far more likely to engage
Crisis becomes less likely — and when it happens, it’s handled earlier and safer
We can do better. And we must.
#MaternalMentalHealth #PaternalMentalHealth #PerinatalMentalHealth #FamilyMentalHealth #EarlyIntervention #WholeFamilyApproach #FathersMatter

The World Is Ignoring Fathers in Global Mental Health Policy
What the World Health Organization Must Get Right About Perinatal Mental Health
The World Health Organization (WHO) has been clear: perinatal mental health matters. Pregnancy and the postnatal period represent a time of heightened psychological vulnerability, with profound consequences for parents, children, and society if mental health needs are not recognised and supported.
And yet, within the world’s leading global health frameworks, fathers are largely missing.
This is not a minor gap. It is a structural omission that undermines prevention, weakens families, and costs lives.
A narrow definition of perinatal mental health
WHO guidance on perinatal mental health overwhelmingly focuses on mothers — understandably, given the biological, medical, and psychological risks women face during pregnancy and childbirth. This work has saved lives and must continue.
But perinatal mental health is not experienced by mothers alone.
Fathers also undergo profound psychological, emotional, and social change during pregnancy and after birth. Research from multiple countries shows that around one in ten new fathers experience depression, with many more experiencing anxiety, trauma, distress, and identity disruption.
For some, this period coincides with financial pressure, sleep deprivation, relationship strain, unresolved trauma, and a powerful expectation to cope silently.
Despite this, fathers remain largely absent from global mental health policy language, screening frameworks, and service design.
If fathers aren’t named, they aren’t supported
Policy language matters.
When fathers are not explicitly recognised in global guidance:
- They are rarely screened for mental health difficulties
- Services are not designed with them in mind
- Data on paternal mental health remains limited and underfunded
- Help-seeking is further discouraged by silence and stigma
This invisibility is not neutral. It reinforces the idea that fathers’ mental health is secondary — or irrelevant — during the perinatal period.
The consequences ripple far beyond men
Ignoring fathers’ mental health does not only harm fathers. It directly affects mothers, babies, and long-term child development.
Evidence consistently links poor paternal mental health with:
- Increased risk of postnatal depression and anxiety in mothers
- Reduced bonding and emotional availability from fathers
- Higher levels of relationship conflict and breakdown
- Poorer emotional, behavioural, and developmental outcomes for children
WHO rightly emphasises prevention, early intervention, and the critical importance of the first 1,001 days of a child’s life. But you cannot protect early child development while ignoring one of the child’s primary caregivers.
A “whole-family approach” that excludes fathers is not whole — it is incomplete.
A global blind spot with global consequences
WHO guidance shapes national policy, commissioning decisions, workforce training, and service models across the world. When fathers are absent from global frameworks, that absence is replicated downstream in health systems everywhere.
The result is a global blind spot:
- Fathers’ distress goes unnoticed
- Suicide risk among new fathers remains hidden
- Preventable harm becomes entrenched
- Families absorb the cost when systems do not
This is not about blaming WHO. It is about recognising the power and responsibility that comes with global leadership.
What the World Health Organization must get right
If WHO is serious about prevention, early intervention, and family wellbeing, then perinatal mental health policy must evolve. That means:
- Explicitly naming fathers in perinatal mental health frameworks
- Recognising paternal mental health as a public health issue, not a secondary concern
- Encouraging routine identification and support for fathers during pregnancy and after birth
- Embedding fathers into whole-family models of care, rather than treating them as peripheral
- Supporting better data collection and research to inform future global guidance
This does not detract from maternal mental health. It strengthens it.
Supporting fathers improves outcomes for mothers. Supporting both parents improves outcomes for children. Supporting families reduces long-term social, economic, and health costs.
Silence is not neutral
Every omission sends a message. And the current message is clear: fathers’ mental health is optional.
It isn’t.
If global mental health policy continues to overlook fathers during the perinatal period, we will continue to see avoidable suffering, fractured families, and lives lost that could have been saved.
Perinatal mental health cannot be considered complete until all parents are seen.
The world’s leading health authority has the opportunity — and the obligation — to lead that change.
References
- World Health Organization. Maternal mental health. WHO.
- World Health Organization. Integration of perinatal mental health into maternal and child health services. WHO, 2022.
- World Health Organization. mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings. WHO.
- Ramchandani P, Stein A, Evans J, O’Connor TG. Paternal depression in the postnatal period and child development: a prospective population study. The Lancet, 2005.
- Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA, 2010.
- Fisher J et al. Prevalence and determinants of common perinatal mental disorders in fathers: systematic review and meta-analysis. Journal of Affective Disorders.
- Gutierrez-Galve L et al. The impact of paternal depression on child development. Child Psychiatry & Human Development.

Failing New Fathers Is Costing the UK Billions Every Year,
A New Economic Report - Fathers Reaching Out
A new economic report from Fathers Reaching Out warns that failing to support new fathers’ mental health is costing the UK at least £10 billion per year, with major financial consequences for workplaces, families, public services, and the wider economy.
The report brings together national research, economic modelling, and lived experience to show that ignoring fathers during pregnancy and early parenthood is not only a human tragedy — but a significant and largely preventable economic failure.
“This is not a niche issue,” said Mark Williams, founder of Fathers Reaching Out.
“Failing new fathers impacts mothers, children, workplaces, and public services. The cost is enormous — and it is avoidable.”
A Hidden Mental Health Crisis
While maternal mental health has rightly gained increased attention, fathers remain largely invisible in perinatal mental health pathways.
Evidence shows many new fathers experience
:
Depression and anxiety
Birth trauma and PTSD
Severe sleep deprivation
Financial and relationship stress
Domestic violence
Yet most fathers are not routinely screened, are rarely asked how they are, and are often excluded from support services.
Research from Swansea University highlights a hidden crisis of suicide among new fathers, with devastating personal and economic consequences.
The Economic Cost of Suicide
Suicide has a significant economic impact beyond the human loss.Government estimates place the cost of each suicide at £1.7–£2 million.Costs include lost productivity, NHS use, emergency services, and long-term social impact.
Preventable deaths among new fathers therefore contribute hundreds of millions of pounds each year.
Workplace Costs: A Hidden Burden
Untreated paternal mental ill-health directly affects UK employers.
Poor mental health already costs UK workplaces over £50 billion per year
Fathers struggling during the perinatal period contribute through:
Sickness absence
Presenteeism (being at work but unwell)
Job loss and long-term economic inactivity
This represents a substantial but often unrecognised part of the national productivity gap.
Relationship Breakdown and Family Costs
Mental ill-health in fathers is strongly linked to relationship stress and breakdown.
Family breakdown costs the UK over £50 billion per year
Poor parental mental health is a major risk factor
Costs arise through housing, benefits, legal processes, social care, and safeguarding services
Supporting fathers early reduces the risk of separation, parental alienation, and long-term family instability.
When a father is unable to maintain contact with their children due to depression, costs often include:
Increased mental health service use (GPs, therapy, medication, crisis support)
Reduced ability to work or job loss
Increased reliance on benefits
Housing instability following separation
Estimated public cost per affected father:
£20,000 – £40,000 per year
(This excludes long-term costs to children.)
Impact on Children and Adverse Childhood Experiences (ACEs)
Children exposed to parental mental ill-health face higher risks of emotional, behavioural, and developmental difficulties.
Research shows:
England & Wales: ACEs cost £42.8 billion per year
Scotland: ACE-related costs estimated at £4–£6 billion per year
Northern Ireland: Population-adjusted estimates suggest £1–£2 billion per year
Total UK ACE-related cost: £48–£51 billion per year.
Poor parental mental health is a key driver of ACE exposure. Supporting fathers early is therefore a powerful form of ACE prevention.
The Overall Cost
When suicide, workplace impact, family breakdown, child development, health services, benefits, and long-term social harm are combined, the report estimates that:
Failing to support new fathers is costing the UK at least £10 billion every year
This figure is considered conservative, as intergenerational and long-term impacts are difficult to fully quantify.
The Solution: Early Prevention
The report outlines a clear and affordable solution.
Estimated cost of effective national support: £300–£600 million per year
Less than 6% of the cost of doing nothing
Estimated return: £15–£30 saved for every £1 invested.
“Early prevention is not a luxury,” Williams said.
“It saves lives, strengthens families, and saves billions every year.”
Calls to Action
Fathers Reaching Out is calling for:
Routine mental health screening for fathers
Inclusion of fathers in perinatal mental health services and universal pathways of care.
Early intervention rather than crisis response
Better workplace policies for new fathers
Read the full Fathers Reaching Out Economic Report.
References / Sources
Swansea University (2023). Hidden crisis of suicide among new fathers in the UK.
Department of Health and Social Care (2017). Preventing suicide in England.
Estimates the economic cost of suicide at £1.7–£2 million per death.
Office for National Statistics (2022–2024).
Suicide rates, mental health, employment and productivity data.
Deloitte (2022).
Mental health and employers: The case for investment.
Estimates workplace mental health costs at £51 billion per year.
Centre for Social Justice (2013; updated estimates).
Fractured families.
Estimates family breakdown costs exceeding £50 billion per year.
MBRRACE-UK (2025).
Saving Lives, Improving Mothers’ Care – Maternal Mental Health Report.
NIHR Applied Research Collaboration (ARC) (2024).
New research suggests fathers need more support in the perinatal period.
Bellis, M.A. et al. (2020).
Health and financial burden of adverse childhood experiences in England and Wales.
The Lancet Public Health, 5(8), e451–e459.
Public Health Scotland / NHS Health Scotland (2019).
Based on ONS, DWP, NHS, OECD and housing sector evidence, untreated paternal depression can cost the public purse £20,000–£40,000 per father per year.
ACE prevalence and economic impact estimates for Scotland.
Public Health Agency Northern Ireland / Department of Health NI (Various).
Trauma, ACE prevalence, and population mental health research informing economic modelling.
Note
All figures are conservative estimates drawn from peer-reviewed research, national statistics, and government-commissioned reports. They are intended to inform public debate and prevention-focused policy.

Failing Fathers: The Hidden Suicide Crisis Missing from NICE Perinatal Mental Health Guidance
In the UK, suicide remains one of the leading causes of death for men under 50. When we look at the perinatal period specifically, the contrast is stark and deeply uncomfortable: for every one mother who dies by suicide, around seven fathers die.
And yet, in 2026, fathers’ mental health during pregnancy and the postnatal period remains largely invisible in national clinical guidance.
The flagship guideline for perinatal mental health in England and Wales — NICE CG192 (Antenatal and postnatal mental health: clinical management and service guidance) — is almost entirely focused on mothers. While maternal mental health absolutely deserves priority and protection, this single-lens approach has created a serious and costly gap.
What NICE CG192 focuses on
NICE CG192 provides comprehensive guidance on identifying, assessing and treating mental health conditions in mothers during pregnancy and after birth. It covers depression, anxiety disorders, post-traumatic stress disorder, bipolar disorder and postpartum psychosis, with clear clinical pathways and service expectations.
This work has saved lives — and continues to do so.
However, fathers, partners and co-parents are not treated as individuals with mental health needs of their own.
Where fathers appear — and where they don’t
Within CG192, fathers are mentioned only occasionally, and almost exclusively:
as a source of support for the mother
as someone who may be involved in her care or treatment plan
as part of the wider family context
There is:
no routine screening for paternal mental health
no guidance on recognising depression, anxiety or trauma in fathers
no referral pathways for distressed dads
no acknowledgement of paternal suicide risk during the perinatal period.
In practice, this means fathers can attend appointments, scans and postnatal visits while experiencing profound distress — and never once be asked how they are coping.
Why this gap matters
Research consistently shows that paternal mental ill-health:
increases the risk of relationship breakdown
affects bonding and attachment
negatively impacts child emotional and behavioural development
raises the likelihood of adverse childhood experiences (ACEs)
Crucially, men are also far less likely to seek help without being directly asked or invited into support.
When guidance fails to recognise fathers, services follow suit.
The result is predictable:
Distress goes unnoticed
Problems escalate
Opportunities for early prevention are missed
The long-term human and economic costs increase
Prevention starts with inclusion
Supporting fathers’ mental health is not about diverting attention away from mothers — it is about strengthening the whole family system.
Early identification and support for dads:
reduces suicide risk
improves outcomes for mothers
protects child development
lowers long-term costs across health, social care, education and justice systems
Ignoring fathers does the opposite.
The bottom line
NICE CG192 primarily focuses on mothers, with only limited mention of partners and new fathers — leaving a significant gap in paternal mental health recognition, assessment and support.
In light of current evidence and suicide statistics, this gap is no longer acceptable.
If we are serious about prevention, we must move beyond seeing fathers as “supporters” only — and start recognising them as parents with mental health needs of their own.
Failing fathers is costing lives. Supporting fathers saves them.
References
National Institute for Health and Care Excellence (2014, updated)
CG192: Antenatal and postnatal mental health – clinical management and service guidance.
NICE, London.
Office for National Statistics (latest available data)
Suicides in the UK.
ONS, UK.
(Shows suicide as one of the leading causes of death for men under 50.)
MBRRACE-UK (latest reports)
Saving Lives, Improving Mothers’ Care.
University of Oxford.
(Maternal suicide data used for comparison.)
Swansea University 2025
Research on male suicide, socioeconomic factors, and life-course risk, including the vulnerability of men during major life transitions such as parenthood.
Ramchandani, P., Stein, A., Evans, J., & O’Connor, T. (2005; 2008).
Paternal depression in the postnatal period and child development outcomes.
Journal of the American Academy of Child & Adolescent Psychiatry / The Lancet.
Wilson, S., Durbin, C. E. (2010).
Effects of paternal depression on fathers’ parenting behaviors.
Clinical Psychology Review.
Felitti, V. J., et al. (1998).
Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults (ACEs study).
American Journal of Preventive Medicine.

The Fatherhood Tree- Mark Williams 2020
Intergenerational Trauma - Paternal Mental Health
The Fatherhood Tree - Mark Williams
Mental Health Early Prevention Begins at Pregnancy:
Intergenerational Fatherhood, Paternal Mental Health, and the First 1001 Days
Abstract
Early mental health prevention is most effective when it begins during pregnancy and the first 1001 days of life. While maternal mental health has increasingly been prioritised, paternal mental health and intergenerational experiences of fatherhood remain under-recognised within prevention strategies.
This paper presents a practice-informed, lived-experience account of how patterns of fathering, emotional availability, and silence around mental health are transmitted across generations. Using The Williams Fatherhood Tree Model (2020), the paper illustrates how survival-based fatherhood can evolve into emotionally attuned fatherhood, and how intentional inclusion of fathers during pregnancy can promote positive intergenerational mental health outcomes. The paper argues for embedding paternal mental health within early prevention and perinatal policy frameworks.
Keywords: paternal mental health; early prevention; intergenerational trauma; fatherhood; first 1001 days; lived experience
1. Introduction
Mental health prevention is frequently framed as an intervention delivered once difficulties emerge. However, evidence increasingly highlights pregnancy and the first 1001 days of life as a critical period for brain development, attachment, and long-term emotional wellbeing. Despite this, fathers are often positioned as peripheral figures within early years policy and practice, resulting in missed opportunities for prevention.
This paper argues that early mental health prevention must explicitly include fathers and attend to intergenerational experiences of fatherhood. Drawing on lived experience, practice-based knowledge, and systems theory, it explores how emotional patterns are passed across generations — and how these patterns can be reshaped through early support.
2. Intergenerational Context and Survival-Based Fatherhood
For many families, fatherhood has historically been shaped by survival rather than emotional expression. In my own family history, my grandfather worked as a coal miner. His primary responsibility was to provide materially — to ensure food was on the table. Emotional availability was constrained by physical labour, economic pressure, and social expectations of masculinity.
These experiences form the roots of what I later conceptualised as The Williams Fatherhood Tree Model (2020). They are not individual failings, but structural and cultural conditions that shaped how fatherhood was enacted and understood.
3. Adaptation Across Generations: What Changed
My father inherited these roots but adapted them. He also worked as a coal miner, yet expanded the role of fatherhood beyond provision. He cooked, cleaned, worked, and spent quality time with me. This represented a significant generational shift from absence to presence.
However, one element remained largely absent: conversations about mental health. Emotional struggles were not named, discussed, or shared. This silence was not intentional; it was inherited.
4. Silence, Crisis, and Late Conversations About Mental Health
Mental health entered our family conversations only later in life, when my father experienced psychosis linked to a severe water infection and calcium imbalance. By this point, distress had already escalated into crisis.
This reflects a broader pattern within men’s mental health, where emotional difficulties are normalised, help-seeking is delayed, and intervention occurs too late. Within the Fatherhood Tree Model, this represents strain placed on the trunk — the father in the present — carrying unresolved pressures from both past experiences and current demands.
5. Becoming a Father With Awareness
When I became a father myself, I carried forward the strengths modelled by my father — presence, care, and responsibility — while also becoming aware of what had been missing: emotional language and openness about mental health.
This awareness shaped my approach to fatherhood and informed my professional practice. I learned that being physically present is not enough; emotional literacy, help-seeking, and open dialogue are critical protective factors
6. The Williams Fatherhood Tree Model (2020)
The Williams Fatherhood Tree Model (2020) conceptualises fatherhood as a dynamic, intergenerational system:
Roots: childhood experiences, trauma, culture, and socio-economic context
Trunk: current mental health, identity, coping strategies, and help-seeking
Branches: roles, relationships, work, and system involvement
Leaves and fruit: child wellbeing, attachment, and long-term outcomes
The model emphasises that trauma can be transmitted across generations, but so can reflection, growth, and healing.
7. Early Prevention and the First 1001 Days
Pregnancy and the first 1001 days represent a unique opportunity for early mental health prevention. When fathers are supported during this period, emotional awareness can develop before crisis occurs, mental health conversations can be normalised, and fathers can model openness for their children.
If my son chooses to become a father, he will inherit not only presence and care, but emotional understanding and permission to talk about mental health. In this way, the intergenerational cycle does not simply break — it becomes progressively more positive.
8. Implications for Policy and Practice
Practice-informed evidence suggests that:
paternal mental health should be embedded within perinatal pathways
fathers must be included in early prevention and 1001 days strategies
intergenerational models should inform commissioning decisions
lived experience should be recognised as valid and valuable knowledge
Early prevention is most effective when it addresses systems, not just symptoms.
9. Conclusion: Prevention as Intergenerational Protection
Mental health prevention begins long before diagnosis, crisis, or service involvement. It begins in pregnancy, within family histories, and in how fathers are supported to understand and express their own mental health.
Early intervention with fathers during the perinatal period has the potential to reduce adverse childhood experiences (ACEs) by addressing unresolved trauma, emotional withdrawal, and relational stress before these patterns become embedded. When fathers receive appropriate support, the risks associated with parental separation, emotional disengagement, and cumulative family strain can be reduced, contributing to greater family stability.
Supporting paternal mental health also plays a crucial role in bonding and attachment. Fathers who are emotionally supported are better able to engage in sensitive caregiving, co-regulation, and the development of secure attachment relationships. These early relational experiences are foundational to children’s emotional development, behavioural regulation, and long-term mental health.
Early prevention further contributes to suicide and mental health prevention across the life course. Many men who later experience severe mental health crisis or suicidal distress report prolonged periods of unsupported emotional difficulty. Normalising mental health conversations during pregnancy and early parenthood creates protective pathways, reduces stigma, and encourages earlier help-seeking among fathers.
The impact on children is both immediate and enduring. Children raised in emotionally attuned, mentally supported family environments are less likely to experience toxic stress, behavioural difficulties, and later mental health problems. By investing in paternal mental health early, services can support healthier childhoods, stronger family relationships, and more resilient future generations.
In this way, early prevention does not simply interrupt harm — it actively builds wellbeing. Supporting fathers early strengthens attachment, reduces adversity, lowers suicide risk, and enables intergenerational cycles to grow increasingly positive over time.
Author Statement
Mark Williams is a mental health campaigner, published author trainer, and founder of Fathers Reaching Out. His work focuses on paternal mental health, early prevention, and systems change informed by lived experience.
Attribution
The Williams Fatherhood Tree Model (2020)
© Mark Williams, 2020
References
Bowen, M. (1978), Family Therapy in Clinical Practice, Jason Aronson, New York, NY.
Bronfenbrenner, U. (1979), The Ecology of Human Development, Harvard University Press, Cambridge, MA
Cabrera, N.J. et al. (2014), “The ecology of father–child relationships”, Journal of Family Theory & Review, Vol. 6 No. 4, pp. 336–354.
Darwin, Z. et al. (2021), “Fathers’ experiences of perinatal mental health support”, BMC Pregnancy and Childbirth, Vol. 21 No. 1.
Felitti, V.J. et al. (1998), “Relationship of childhood abuse and household dysfunction”, American Journal of Preventive Medicine, Vol. 14 No. 4, pp. 245–258.
Fonagy, P. et al. (2002), Affect Regulation, Mentalization and the Development of the Self, Other Press, New York, NY.
Goodman, J.H. (2004), “Paternal postpartum depression”, Journal of Advanced Nursing, Vol. 45 No. 1, pp. 26–35.
Lamb, M.E. (2010), The Role of the Father in Child Development (5th ed.), Wiley, Hoboken, NJ.
Shonkoff, J.P. et al. (2012), “The lifelong effects of early childhood adversity and toxic stress”, Pediatrics, Vol. 129 No. 1, pp. e232–e246.
Williams, M. (2020), The Williams Fatherhood Tree Model, Fathers Reaching Out, Wales, UK.
The 1001 Critical Days (2021), Building the Foundations for Lifelong Mental Health, UK
